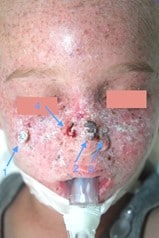
Case
A four-year-old boy was referred to the Dermatology department of Ghent University Hospital after excision of a keratoacanthoma on the dorsum of the nose. Extensive facial dyskeratoses, manifest facial freckling, conjunctival injection and photophobia were observed during patient examination. Four facial lesions were suspicious for malignancy. Photodamage was also present on other sun-exposed areas, but to a lesser extent (dorsum of the hands, neck, lower arms and legs). When he was a baby, his parents noticed that their son tanned quickly. Freckling started at the age of one. His neurological development was normal. Family history is negative for skin cancer or consanguinity. Altogether, this clinical picture was suggestive for a DNA-repair disorder and more specifically xeroderma pigmentosum (XP). Genetic testing is ongoing and results will be known early 2021. We present the treatment of our patient and the current knowledge on management of this disease.
To refresh your memory: what is xeroderma pigmentosum?
XP is a rare, photosensitive disease which is inherited in an autosomal recessive manner. The estimated incidence in Western Europe is 2,3 per million live births. XP-patients have a defect in the repairing mechanisms for ultraviolet radiation (UV) – induced DNA damage. The disease is classified into eight subtypes, each with a separate responsible gene and various clinical manifestations. The earliest features are extreme sun-sensitivity, followed by skin aging and multiple skin cancers at a later age. Neurological abnormalities may be present in a quarter of patients. It is estimated that XP patients have a 10,000-fold increased risk of non-melanoma skin cancer and a 2,000-fold increased risk of melanoma under the age of 20. According to the subtype, there is an approximately 50-fold increase in internal neoplasms, especially of the central nervous system 1–3. A 39-year follow-up study (1971-2009) found skin cancer to be the most common cause of death with 45% of the patients living into their 40’s. The prognosis is significantly worse for patients with neurodegeneration 4. They commonly die of aspiration, infection or trauma at approximately 30 years-of-age 5.
Principles in the management of xeroderma pigmentosum
The management of cutaneous XP manifestations is mainly based on two principles: rigorous UV-protection in order to prevent further photodamage and adequate treatment of precancerous lesions and skin tumours. UV protection is threefold and includes (1) avoidance of sun-exposure outside, as well as indoors by means of UV-blocking films on windows and correct indoor lighting; (2) protective clothing and sunglasses and (3) regular application of sunscreens. Photodynamic therapy, systemic acitretin, nicotinamide, cryotherapy, electrosurgery, topical imiquimod and 5-fluoruracil may be used to treat precancerous lesions, even though evidence in young children is limited. Surgery needs to be performed in a tissue-sparing manner due to the high number of tumours that may occur in neighbouring sites. A regular ophthalmology and ear-nose-throat (ENT) check-up is warranted 1–3.
Management applied to our patient
Mapping of the suspicious lesions by means of punch biopsies under general anaesthesia identified three keratoacanthoma-like squamous cell carcinomas and one basal cell carcinoma (Fig. 1). In a second procedure, these malignancies were surgically removed and the surrounding actinic keratosis were treated with cryotherapy. The surgical defect was temporarily covered with donor skin awaiting the histologic results. Two more sessions took place until free histologic margins were obtained (slow Mohs procedure). Next, the surgical defect was covered with an autologous split-thickness skin graft taken from non-sun exposed gluteal skin on top of Glyaderm®, a dermal substitute (Fig. 2). Staging by cervical ultrasound revealed an adenopathy at the right supraclavicular region. A fine needle aspiration took place during the surgical procedure and did not reveal any malignancy. In addition, blood samples, ENT and ophthalmology review were performed during this anaesthesia. Two weeks after the last surgical session, good healing of the skin graft was seen, but crusted lesions emerged in the surrounding areas. Additional preventive systemic therapy with acitretine was initiated and the patient is planned for a new multidisciplinary consultation.


Conclusion
XP is a rare entity in the field of paediatric dermatology, for which management is multidisciplinary and challenging. In order to improve the prognosis, drastic UV protection and early treatment of skin tumours is essential. We present the therapeutic approach of XP by means of a case that we recently encountered in our practice.
References
- Lehmann AR, Mcgibbon D, Stefanini M. Xeroderma pigmentosum. Orphanet J Rare Dis. 2011;6(70):1–6.
- Black JO. Xeroderma Pigmentosum. Head Neck Pathol. 2016;10(2):139–44.
- Zghal M, Fazaa B, Abdelhak S, Mokni M. Xeroderma pigmentosum. Ann Dermatol Venereol. 2018;145(11):706–22.
- Bradford P, Goldstein A, Tamura D, Khan S, Ueda T, Boyle J, et al. Cancer and neurologic degeneration in xeroderma pigmentosum: long term follow-up characterizes the role of DNA repair. J Med Genet. 2011;48(3):168–76.
- Moriwaki S, Kanda F, Hayashi M, Yamashita D. Xeroderma pigmentosum clinical practice guidelines. 2017;125(April):2013–22.
Authors: Dr. Genouw E. (1), Prof. Dr. Brochez L. (1,2), Dr. Dhooghe N. (3), Prof. Dr. De Schepper S. (1)
(1) Ghent University Hospital, Dermatology Department
(2) Cancer Research Institute Ghent (CRIG)
(3) Ghent University Hospital, Plastic Surgery Department